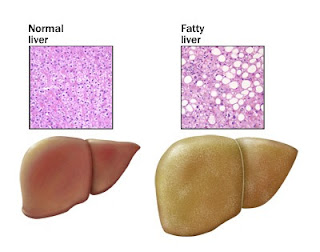
Los Angeles, Calif - Two studies from the Childhood Obesity Research Center at the Keck School of Medicine of the University of Southern California (USC) have found evidence that Hispanic children and adolescents are genetically predisposed to developing fatty liver disease--a condition that can lead to cirrhosis, cardiovascular disease and diabetes.
The studies, recently published in the journals Diabetes and the American Journal of Clinical Nutrition, found that Hispanic children who carry the PNPLA3 gene variant (GG) have increased liver fat. Children who carry the variant are also more susceptible to developing liver fat when consuming a high sugar diet.
Previous research has shown that Hispanics are particularly susceptible to the accumulation of fat in the liver, and reports suggest that nearly four of 10 obese Hispanic children and adolescents have nonalcoholic fatty liver disease (NAFLD).
"Collectively these findings demonstrate that Hispanics are genetically susceptible to the negative health effects of high sugar consumption, and that this effect is manifested early in life," said Principal Investigator Michael I. Goran, professor of preventive medicine, physiology and biophysics and pediatrics, and director of the USC Childhood Obesity Research Center at the Keck School of Medicine. "This is a major public health concern, especially in the face of massive marketing of sugary beverages to children."
The researchers conducted cross-sectional studies of more than 300 Hispanic youth (ages 8-18) in the Los Angeles area, using metabolic, diet and genetic measures. They found that GG carriers have almost double the amount of liver fat content as non-carriers. The effects are strongest in Hispanics because the frequency of the variant is much higher (49%) than in whites (23%) or African Americans (17%), said Jaimie Davis, assistant professor of preventive medicine at the Keck School of Medicine, and a lead author on the studies.
The findings suggest that obese Hispanic children with the variant have an increased capacity for fat storage and decreased hepatic lipid mobilization (breakdown of stored fats), among those whose diets are high in sugar, she said.
Sugar intake is high among youth in Los Angeles, and accounts for nearly half of all daily carbohydrate intake and 25 percent of energy intake. However, because the link between high sugar diets and liver fat accumulation was only evident among children who had the GG variant, the findings could have important implications for treating NAFLD, Davis said.
"Specific dietary interventions based on the genetic predisposition may lead to more effective therapeutic outcomes in children with fatty liver disease," she said. "I think the studies really highlight the need to test such diet and genotyping interventions."
The work done by Dr. Goran and his team is at the interface of personalized and community health, said D. Brent Polk, M.D., professor and chair of the Department of Pediatrics and director of the Saban Research Institute at the Keck School of Medicine and Childrens Hospital Los Angeles.
"While we know that this genetic variant is overrepresented in Hispanic people, the findings help us identify individuals with increased susceptibility to worse disease," he said. "Now we can ask does early intervention in this group prevent their progression to the complications of fatty liver disease?"
The studies were supported by the National Institute of Cancer, University of Southern California Center for Transdisciplinary Research on Energetics and Cancer, the National Institute of Child Health and Human Development, the Minority Research Center of Excellence, the National Heart, Lung, and Blood Institute, the Dr. Robert C. and Veronica Atkins Foundation, the National Institute of Diabetes and Digestive and Kidney Diseases, and the MGM Mirage Fund at the University of Southern California.